FP/RH 2030 – what might Ethiopia’s family planning/reproductive health landscape be like in the coming years?
In a country known for ambitious planning and achievement, what will the family planning / reproductive health (FP/RH) landscape look like in the future? Below are a few possibilities that may define the coming years.
STORIED PAST
Ethiopia’s success in setting and achieving ambitious FP and RH targets is well known. The country was a leader in Africa in Millennium Development Goal (MDG) achievement and was one of two countries selected for an EXCELL award at the 2016 International Conference on Family Planning in Indonesia.

LONG-TERM METHODS
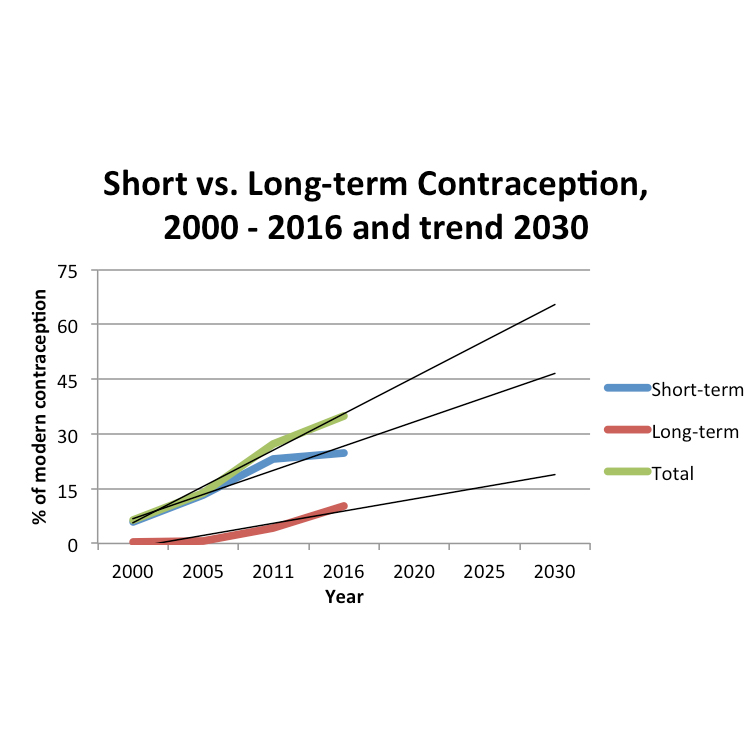
The growth in long-acting reversible contraception (LARC) as a share of overall contraception is a notable feature of recent FP data.
In 2000, long-term methods accounted for 6% of modern family planning in Ethiopia. By 2016, this figure had increased to 29% (2016 Ethiopian Demographic and Health Survey Key Indicators Report).
Extrapolating from recent DHS surveys suggests that roughly 20% of married women 15 – 49 years of age will be using LARCs in 2030 and approximately 45% using short-term methods.

Currently, married women 15 – 49; Source: EDHS Surveys 2000 – 2011, Key Indicators Report 2016
Likely, this ratio underestimates the impact of recent efforts to prioritize LARCs[1]. User-friendly and cost-effective products like Implanon NXT and the post-partum intra-uterine device (PPIUD) promise additional growth of these methods.
The significant cost-advantages of LARCs are likely to drive procurement and policy priorities in the coming years. The GoE estimates that an IUD costs $0.19 per couples year protection (CYP) compared to $1.50 for pills and $5.00 for injectable contraceptives[2]. Implant contraceptives, one form of LARC, are on the more expensive side at $4.31 per CYP, suggesting IUDs may ultimately prevail as the LARC of choice.
HIV VACCINE
Researchers estimate that HIV prevention and treatment will cost US$98 – $261 billion for 2015–2050 in the nine countries in Africa most affected by HIV[3], a group that includes Ethiopia. At the same time, donor support for HIV interventions in low and middle-income countries is slowing[4].
Could a vaccine be the solution?
A National Institutes of Health (NIH)-supported clinical trial led by the HIV-Vaccine Trials Network (HVTN) is testing whether a new version of the RV144 HIV-vaccine candidate safely prevents HIV infection among South African adults[5]. The RV144 HIV vaccine candidate is the only candidate to have shown some protection against HIV.
Ethiopia has projected AIDS expenditures of roughly $460 million annually from 2015 – 2018[6]. In this context, a cost-effective vaccine could make a significant economic as well as humanitarian impact.
PHARMACEUTICAL MANUFACTURING
Ethiopia has over 200 pharmaceutical and medical importers and just nine local manufacturers involved directly in the manufacture of pharmaceuticals, who, combined, are able to reach only 20% of the local market[7].
The National Strategy and Plan of Action for Pharmaceutical Manufacturing Development in Ethiopia (2015–2025) seeks to catalyse growth in the pharmaceutical sector, which is expected to reach $1 billion in 2018 and is growing by 25% per annum.
Could Ethiopia’s FP and RH needs be met through local manufacture?
One factor that will likely assist is the country’s rapid growth in academic research and tertiary education.
The exponential growth of universities over the past two decades[8] means that Ethiopia has a considerable pool of human talent from which to build a manufacturing base. Academic partnerships in the form of public-private partnerships can potentially buffer high capital requirements to pharmaceutical development.
References
2. Federal Ministry of Health [Ethiopia]. Costed Implementation Plan for Family Planning in Ethiopia, 2015/16–2020; 2016.
3. Atun R, Chang AY, Ogbuoji O, et al. Long-term financing needs for HIV control in sub-Saharan Africa in 2015–2050: A modeling study. BMJ Open. 2016;6(3):e009656. doi:10.1136/bmjopen-2015-009656.
4. AVERT. Funding for HIV and AIDS. https://www.avert.org/professionals/hiv-around-world/global-response/funding. Published 2015. Accessed May 25, 2017.
5. HIV Vaccine Trials Network. HIV Vaccine Trials Network – Scientific Achievements. http://www.hvtn.org/en/about/scientific-achievements.html. Accessed May 25, 2017.
6. Resch S, Ryckman T, Hecht R. Funding AIDS programmes in the era of shared responsibility: An analysis of domestic spending in 12 low-income and middle-income countries (Supplement). Lancet Glob Heal. 2014.
7. Ministry of Health and Ministry of Industry of Ethiopia. National Strategy and Plan of Action for Pharmaceutical Manufacturing Development in Ethiopia (2015 – 2025 ): Developing the Pharmaceutical Industry and Improving Access; 2015.
8. Woldegiyorgis AA. A Glance at the Ethiopian Higher Education from the Developmental State Perspective. Vol 15.; 2015.